why is obesity more dangerous for men than women?
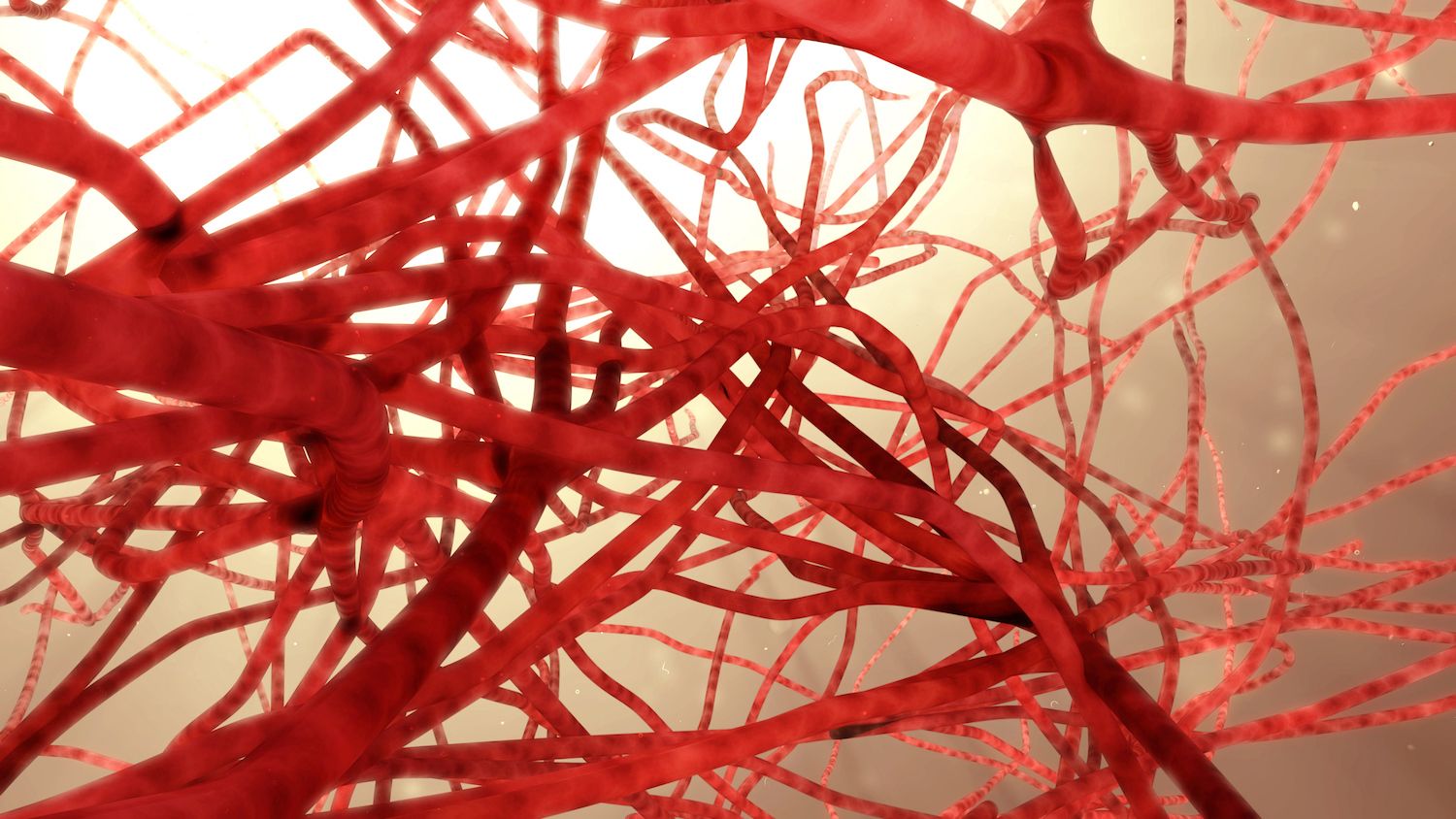
obesity-related conditions like cardiovascular disease and diabetes are more likely to appear in men than women.
what it feels like: 'i've learned to take back control' of obesity
tanya bender says she first noticed her weight when she was 12. she was growing up, her body was changing and, while she was a bit bigger than the other girls in her school, she was not overweight.
living with obesity: 'love yourself, no matter what size you are'
after a lifetime of struggling with weight and feeling badly about herself, patricia eagles has some important advice to share — mostly that there is always hope for recovery.
 4 minute read
4 minute read