asthma in children
condition basics
what is asthma?
asthma is a lung disease that makes it hard for your child to breathe. it causes the airways that lead to the lungs to swell and get inflamed.
some children have breathing problems only at certain times, like during allergy season, or when they get a cold, or when they exercise. others have breathing problems a lot of the time.
when asthma symptoms suddenly get worse (or flare up), the airways tighten and get narrower. these flare-ups are also called asthma attacks or exacerbations (say "ig-zas-ur-bay-shuns").
treatment can help your child feel and breathe better and help keep your child's lungs healthy. many children with asthma play sports and live healthy, active lives.
what causes it?
experts don't know exactly what causes asthma in children. but we do know that asthma runs in families. and it's much more common in children who have allergies.
what are the symptoms?
when your child has asthma, he or she may wheeze or cough a lot. your child may also feel tightness in the chest or feel short of breath.
how is it diagnosed?
to find out if your child has asthma, your doctor will do a physical exam and ask about your child's symptoms and health. the doctor may also have your child do breathing tests to find out how well your child's lungs work.
how is asthma treated?
asthma is treated with medicine to help your child breathe easier. daily controller medicine is used to prevent asthma attacks. quick-relief medicine is for times when symptoms need to be treated fast. treatment also includes helping your child to avoid things that might trigger symptoms and to follow an asthma action plan.
how can you help your child manage asthma?
you can help your child manage asthma by making sure your child takes asthma medicines the right way, follows an action plan, and avoids things that make asthma worse, like pet dander and dust mites. and you can help your child avoid getting sick by making sure your child gets covid-19 and influenza (flu) vaccines.
health tools
health tools help you make wise health decisions or take action to improve your health.
decision points focus on key medical care decisions that are important to many health problems.
actionsets are designed to help people take an active role in managing a health condition.
what increases your risk
your child may be more likely to have asthma if:
- someone in your family has asthma.
asthma may run in families (be inherited). if this is the case in your family, your child may be more likely than other children to get long-lasting (chronic) inflammation in the airways.
- your child or someone in your family has an allergy, including food allergies.
children who have an allergy are more likely than other children to get asthma, though not every child with allergies gets asthma. and not every child with asthma has allergies.
most children with asthma have allergic rhinitis, atopic dermatitis, or both. having atopic dermatitis as a child may also increase the risk of a person having more severe and persistent asthma as an adult.
- your child had respiratory syncytial virus (rsv) and wheezing at a young age.
early infection with respiratory syncytial virus that causes a lower respiratory infection increases a child's risk for wheezing. young children who wheeze have a greater risk for asthma than children who do not wheeze.
- your child's airways overreact.
children who inherit a tendency of the airways (bronchial tubes) to overreact often get asthma.
other risk factors
other things that may put your child at risk for asthma include:
- second-hand cigarette smoke.
children who are around second-hand cigarette smoke are at increased risk for getting asthma. if children already have asthma, second-hand smoke makes their symptoms worse.
- cigarette smoking.
children who smoke are more likely to get asthma when they become teenagers.
- cigarette smoking during pregnancy.
women who smoke during pregnancy increase the risk of wheezing in their babies. babies whose mothers smoked during pregnancy also have worse lung function than babies whose mothers did not smoke.
- obesity.
there is a link between obesity in children and asthma. but the reason for the link is unclear. also, symptoms caused by obesity are sometimes thought to be asthma symptoms.
- exposure to allergens.
being exposed to allergens such as dust mites, cockroaches, and pet dander may increase a child's risk for asthma.
- environment.
environmental factors, such as pollution or dust, may play a role in the development of asthma. exposure to these things may cause children's immune systems to develop in a way that makes it more likely they will develop allergies or asthma.
risks for very bad asthma attacks
your child may be at increased risk for very bad asthma attacks if he or she:
- is an infant with asthma symptoms.
- has a history of very bad symptoms, such as asthma attacks that get worse quickly and frequent nighttime symptoms.
- has a hard time taking medicines or often has to use quick-relief medicines (short-acting beta2-agonists) such as salbutamol.
- has frequent changes in peak expiratory flow.
- has symptoms that last for a long time.
- doesn't use oral steroid medicines soon enough during an attack.
- doesn't have good support from family and friends.
triggers, such as air pollution, pollen, pet dander, and colds and influenza (flu), also may make asthma worse and may lead to asthma attacks.
symptoms
when your child has asthma, your child may:
- wheeze. this is a loud or soft whistling noise when breathing in and out. it happens when the airways of the lungs narrow.
- cough a lot. this is the only symptom for some children.
- feel tightness in the chest.
- feel short of breath. your child may have rapid, shallow breathing or trouble breathing.
- have trouble sleeping because of coughing and wheezing.
- get tired quickly during exercise.
if your child has only one or two of these symptoms, it doesn't always mean that your child has asthma. the more of these symptoms your child has, the more likely it is that your child has asthma.
symptoms of asthma can be mild or severe. your child may have symptoms every day, just now and then, or somewhere in between.
your child might have symptoms right after being exposed to things like pollen or cigarette smoke. this is known as an early phase response. it's also possible that your child's symptoms will start hours after exposure. this is known as a late phase response. it can make it harder to know what things are causing your child's symptoms.
many children have symptoms that get worse at night. in all people, lung function changes throughout the day and night. in children with asthma, this often is very noticeable, especially at night. in these children, a nighttime cough and shortness of breath occur often. in general, waking at night because of shortness of breath or a cough is a sign that asthma needs more treatment. getting treatment can help your child avoid an asthma attack.
learn more
what happens
your child may have symptoms every day, just now and then, or somewhere in between. sometimes your child's symptoms may suddenly get worse (or flare up) and cause an asthma attack. over time, your child's breathing problems may get more severe. or your child may have symptoms more often.
your child may have a hard time breathing only at certain times. this may be during allergy season, when your child gets a cold, or while exercising. or your child may have breathing problems a lot of the time. the things that make your child's asthma or breathing worse are called triggers.
at times, the inflammation from asthma causes your child's airways to narrow and produce mucus. this causes asthma symptoms such as shortness of breath.
even mild asthma may cause long-term changes to your child's airways and lungs. it may speed up and make worse the natural decrease in lung function that occurs as we age. asthma can make lung and airway infections like bronchitis and pneumonia worse.
loss of lung function in asthma appears to start early in childhood. asthma also may increase the risk of a partial collapse of lung tissue (atelectasis) or a collapsed lung (pneumothorax).
treatment can help your child feel and breathe better and help keep your child's lungs healthy. many children with asthma play sports, and most live healthy, active lives.
learn more
watch
when to call a doctor
call 911 or other emergency services immediately if:
- your child is having severe difficulty breathing. signs of this include:
- breathing very fast. children usually grunt with each breath. shortness of breath can interfere with the ability to speak smoothly.
- appearing anxious and being unable to eat because it's too hard to breathe.
- using the neck, chest, and belly muscles to breathe so that the skin between, above, and under the ribs sinks inward with each breath. the nostrils may open wide when your child breathes in.
- taking longer than usual to breathe out and sometimes having a high-pitched, musical sound when breathing in.
- sitting up, leaning forward, or sitting with the nose tilted up as if sniffing the air.
- having skin colour that stays pale, grey, bluish, or mottled, including the tongue, lips, earlobes, and nail beds.
call your doctor now or seek immediate medical care if:
- your child's symptoms do not get better after you follow your child's asthma action plan.
- your child has new or worse trouble breathing.
- your child's coughing and wheezing get worse.
- your child coughs up dark brown or bloody mucus (sputum).
- your child has a new or higher fever.
call your doctor if:
- your child needs to use quick-relief medicine on more than 2 days a week within a month (unless it is just for exercise).
- your child coughs more deeply or more often, especially if there is more mucus or a change in the colour of the mucus.
- your child has asthma and their pef has been getting worse for 2 to 3 days.
if you think your child has asthma
if your child has not been diagnosed with asthma but has asthma symptoms, call your doctor and make an appointment to have your child checked.
watchful waiting
watchful waiting is a wait-and-see approach. it may be okay as long as your child follows their asthma action plan and stays within the green zone. monitor your child's symptoms, and continue to avoid asthma triggers.
exams and tests
to find out if your child has asthma, your doctor will do a physical exam and ask about your child's symptoms. the doctor may also have your child do breathing (lung function) tests. these tests find out how well your child's lungs work.
diagnosing asthma in babies and toddlers is often very hard. symptoms may be the same as those of other diseases, such as infection with respiratory syncytial virus (rsv) or inflammation of the lungs (pneumonia), sinuses (sinusitis), and small airways (bronchiolitis). if you have a very young child, a test such as spirometry isn't practical. so the diagnosis is made based on your report of symptoms.
breathing (lung function) tests
in an older child, lung function tests can help the doctor diagnose asthma, see how bad it is, and check for problems. the tests include:
- spirometry.
doctors use this test to diagnose and keep track of asthma in children age 5 and older. it measures how quickly your child can move air in and out of the lungs and how much air is moved. spirometry is not used with babies and small children. in those cases, the doctor usually will listen for wheezing and will ask how often the child wheezes or coughs.
- peak expiratory flow.
this test shows how much air your child can quickly breathe out using the greatest effort. testing of daytime changes in your child's peak flow may be done over 1 to 2 weeks. this test may help when your child has symptoms now and then but the spirometry test results are normal.
- an exercise or inhalation challenge.
this test measures how well your child can breathe in and out after exercise or after taking a medicine. it may be used if the spirometry test results have been normal or near normal but asthma is still suspected. an inhalation challenge also may be done using a specific irritant or allergen.
tests for other diseases
asthma can be hard to diagnose because the symptoms vary widely from child to child and within each child over time. and asthma-like symptoms can also be caused by other conditions, such as influenza (flu) or other viral lung infections. so your doctor may want to do other tests.
tests that may be done to find out if diseases other than asthma are causing your child's symptoms include:
- a chest x-ray.
this may be used to look for signs of other lung diseases.
- a sweat test.
this measures the amount of salt in sweat. this test may be used to see if cystic fibrosis is causing symptoms.
- bronchoscopy.
this test can be done to examine the airways for problems such as tumours or foreign objects, which can create symptoms that mimic those of asthma. this test uses a long, thin, lighted tube to look at your child's airways.
other tests may be done to see if your child has health problems such as sinusitis, nasal polyps, or gastroesophageal reflux disease.
if your doctor thinks your child's symptoms may be caused by allergies, the doctor may order allergy tests.
learn more
watch
treatment overview
asthma is treated with medicine to help your child breathe easier, along with self-care. other treatments, like counselling, may also be used.
it's very important to treat your child's asthma, even if your child feels good most of the time. that's because mild asthma may also cause changes to the airways that speed up and make worse the natural decrease in lung function that occurs as we age.
babies and small children need early treatment for asthma symptoms to prevent severe breathing problems. they may have more serious problems than adults because their bronchial tubes are smaller.
by following your child's treatment plan, you can help your child meet these goals:
- increase lung function by treating the inflammation in the lungs.
- reduce how often your child has asthma attacks, how long they last, and how bad they get.
- treat the attacks as they occur.
- have a full life by preventing and managing symptoms. this means being able to take part in all daily activities, including school, exercise, and recreation.
- sleep through the night undisturbed by asthma symptoms.
medicines
most medicines for asthma are inhaled. these types of medicines go straight to your child's airways, where the problem is.
the main medicines used to treat asthma include:
- daily controller medicines.
these medicines prevent asthma attacks, help stop problems before they happen, and reduce inflammation in your child's lungs. these things help control your child's asthma.
inhaled corticosteroids are the preferred controller medicines. the controller inhaler may also include a long-acting medicine that relaxes the airways to help your child breathe. your child takes them every day.
- quick-relief medicines.
these medicines are used when symptoms can't be prevented and need to be treated fast. talk to your doctor if your child needs their quick-relief medicine more than 2 days a week within a month.
they help relax the airways and allow your child to breathe easier. salbutamol is a quick-relief medicine that is often used. in some cases, a certain type of controller inhaler is used as a quick-relief medicine. ask your child's doctor what to use for quick relief.
- oral or injected corticosteroids.
these medicines are often used to treat asthma attacks.
other medicines may be given in some cases.
your child needs to have regular checkups to keep asthma under control and to ensure the right treatment. how often your child needs checkups depends on how well the asthma is controlled.
self-care
treatment also includes things you can help your child do to manage asthma, like avoiding things that might trigger symptoms and following an asthma action plan.
other treatments
other treatments may be used to treat asthma. they include:
- counselling.
in addition to taking medicines, counselling may be helpful for children who have asthma. therapy can help to improve anxiety triggers and learn how to manage stress.
- complementary medicine.
complementary medicine is a term used for a wide variety of health care practices that may be used along with standard medical treatment.
while most mind and body practices such as breathing exercises and yoga seem to be safe when used in the right way, be sure to check with your child's doctor first. talk about any complementary health practice that you would like your child to try or that your child is already using. your doctor can help you manage your child's health better if they have the whole picture about your child's health.
- immunotherapy.
if your child has asthma symptoms that are triggered by allergens, the doctor may recommend immunotherapy. for this treatment, your child gets shots that have a small amount of certain allergens in them. your child's body "gets used to" the allergen, so your child reacts less to it over time. this kind of treatment may help prevent or reduce some allergy symptoms.
allergy shots have been shown to reduce asthma symptoms and the need for medicines in some people. but allergy shots don't work equally well for all allergens. these shots should not be given when asthma is not well-controlled.
learn more
caring for your child
there are things you can help your child do to manage asthma.
taking medicines
make sure that your child:
- takes controller medicine to treat inflammation every day not just when your child has symptoms. controller medicine usually includes an inhaled corticosteroid. the goal is to prevent problems before they start.
- uses quick-relief medicine when your child has symptoms of an asthma attack. salbutamol is a quick-relief medicine that is often used. some children need to use quick-relief medicine before they exercise.
- if your child's doctor prescribed corticosteroid pills to use during an asthma attack, make sure your child takes them as directed. they may take hours to work. but they may shorten the attack and help your child breathe better.
- keeps quick-relief medicine with them at all times.
- learns how to use their inhalers the right way. ask your doctor or pharmacist for help.
avoiding triggers
common triggers include colds, smoke, air pollution, dust or dust mites, pollen, mould, pet dander, cockroaches, stress, and cold, dry air. here are some ways you can help your child avoid triggers:
- don't expose your child to cigarette smoke. tobacco smoke is a major cause of asthma symptoms in children.
- keep your child inside when air pollution levels are high.
- help your child avoid infections such as covid-19, colds, and influenza (flu). have your child wash their hands often. talk to your doctor about having your child get the flu vaccine. be sure your child stays up to date on their covid-19 vaccines.
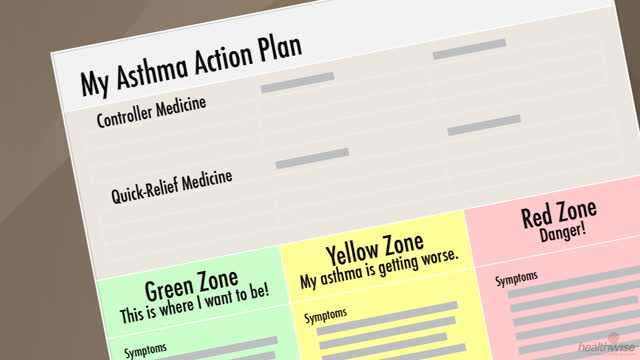
following an asthma action plan
you can help your child follow their asthma action plan. this is a written plan that will help your child manage asthma every day and know what to do during an asthma attack. a plan also helps you and your child make quick decisions about medicine and treatment. if your child doesn't have an action plan, work with your doctor to make one.
monitoring symptoms
if your child is old enough to understand the process, teach your child what symptoms to watch for. and help your child understand how to follow their asthma action plan.
you can monitor your child's symptoms by watching for changes in how much your child is coughing, wheezing, or short of breath. if your child is old enough to understand what to do, you can monitor your child's symptoms by checking their peak expiratory flow (if your doctor recommends that you do this).
measuring peak flow is a way to keep track of asthma symptoms at home. it can help you and your child know when lung function is getting worse before it drops to a dangerously low level. this is done with a peak flow meter.
it's easy to underestimate how bad your child's symptoms are. you may not notice them until your child's lungs are functioning at 50% of the personal best peak expiratory flow.
learn more
watch
medicines
medicine helps your child breathe easier and control their asthma. it doesn't cure asthma. but it's an important part of managing asthma in your child. medicines for asthma treatment are used to:
- prevent and control airway inflammation. this is so your child has fewer asthma symptoms.
- reduce how often your child has asthma attacks, how long they last, and how bad they get.
- treat the attacks as they occur.
most medicines for asthma are inhaled. they allow a certain dose to be given directly to the airways.
most doctors recommend that every child who uses a metered-dose inhaler (mdi) also use a spacer. the spacer is attached to the mdi. a mask spacer has a face mask that fits over your child's mouth and nose. young children who have trouble using their inhalers can use a mask spacer. a spacer may deliver the medicine to your child's lungs better than an inhaler alone. and for many people, a spacer is easier to use than an mdi alone. using a spacer with inhaled steroid (corticosteroid) medicines can help reduce their side effects and the need for the oral (pill) kind.
try to avoid giving your child an inhaled medicine when your child is crying. when a child cries, not as much medicine is delivered to the lungs.
medicine choices
the main medicines used to treat asthma include:
- daily controller medicines.
these medicines prevent asthma attacks, help stop problems before they happen, and reduce inflammation in your child's lungs. these things help control your child's asthma.
inhaled corticosteroids are the preferred controller medicines. your child takes them every day. they include beclomethasone, budesonide, and fluticasone.
- quick-relief medicines.
these medicines are used when symptoms can't be prevented and need to be treated fast. talk to your doctor if your child needs their quick-relief medicine more than 2 days a week within a month.
quick-relief medicines, such as beta2- agonists, help relax the airways and allow your child to breathe easier. salbutamol is a quick-relief medicine that is often used. in some cases, a certain type of controller inhaler is used as a quick-relief medicine. ask your child's doctor what to use for quick relief.
- oral or injected steroid medicines (systemic corticosteroid medicines).
these medicines may be used to treat asthma attacks. they include dexamethasone, prednisolone, and prednisone.
there are other long-term medicines that are sometimes used alone or with other medicines for daily treatment. they include:
- anticholinergics (such as tiotropium). they treat asthma that's not well controlled.
- leukotriene pathway modifiers. an example is montelukast.
- long-acting beta2-agonists. they are always used with an inhaled corticosteroid medicine. they include formoterol and salmeterol.
how your doctor prescribes asthma medicines
medicine treatment for asthma depends on your child's age and type of asthma. it also depends on how well the treatment is helping asthma symptoms.
- children up to age 4 are usually treated a little differently than those 5 to 11 years old.
- the least amount of medicine that controls your child's symptoms is used.
- the amount of medicine and number of medicines are increased in steps. so if your child's asthma isn't controlled at a low dose of one controller medicine, your doctor may raise the dose or add another medicine.
- if your child's asthma has been under control for several months at a certain dose, the doctor may reduce the dose. this can help find the least amount of medicine that will control your child's asthma.
- quick-relief medicine is used to treat asthma attacks. but if your child needs to use it more than 2 days a week within a month, your doctor may change the amount and number of these medicines.
learn more
watch
 asthma: helping a young child take medicine
asthma: helping a young child take medicine asthma: is your child using the quick-relief inhaler too often?
asthma: is your child using the quick-relief inhaler too often? asthma: myths about inhaled steroids
asthma: myths about inhaled steroids asthma: the importance of controller medicines
asthma: the importance of controller medicines how to use a nebulizer with a mask
how to use a nebulizer with a mask long-acting bronchodilators for your child
long-acting bronchodilators for your child helping your child use a metered-dose inhaler with a spacer
helping your child use a metered-dose inhaler with a spacer helping your child use a metered-dose inhaler without a spacer
helping your child use a metered-dose inhaler without a spacer helping your child use a metered-dose inhaler with a mask spacer
helping your child use a metered-dose inhaler with a mask spacer
credits
current as of: august 6, 2023
author: healthwise staff
clinical review board
all healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
current as of: august 6, 2023
author: healthwise staff
clinical review board
all healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.