“i went into that appointment, not feeling there is anything grave at all. i was about to turn 53 and things get a little creaky all around as we’re aging,” he says. “i remember distinctly, she said, ‘you know, there’s something up and we’ll get to the bottom of it.’” he left the appointment with a requisition for an abdominal ultrasound and blood work to test for a broad range of indicators to identify the problem.
this was the first of many steps toward his survival. one of the hurdles in pancreatic cancer is the lack of knowledge about the warning signs like back pain, jaundice and gastrointestinal discomfort. awareness of these could speed up diagnosis and change outcomes.
“not to take this lightly, because i think a lot of doctors would just give dan something digestive and send him on his way based on how he was explaining his symptoms,” kathy says. “so the fact that she said she’s going to get to the bottom of it and she made that ultrasound requisition is a very critical part of dan’s story, because if he had gone any longer we would probably not be where we are today.”
early detection still a missing piece of the puzzle
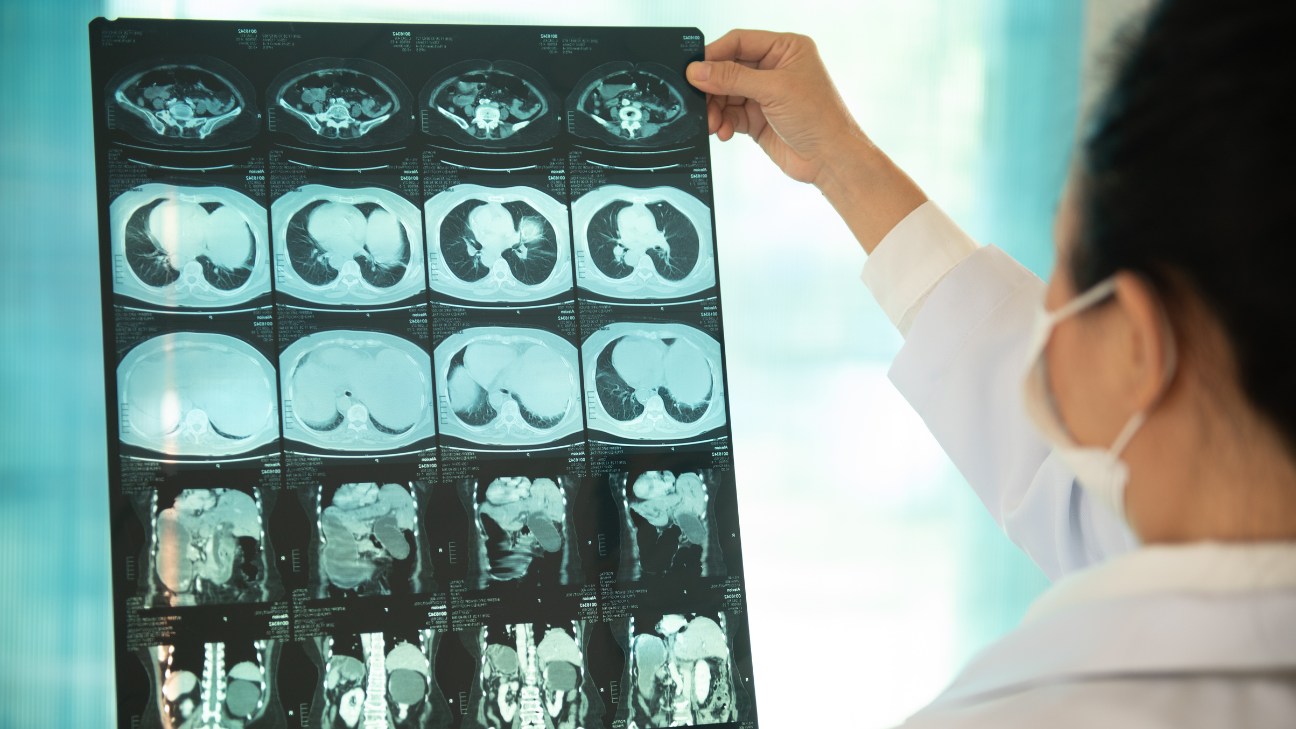
dr. anish kirpalani, chief of radiology at st. michael’s hospital in toronto, specializes in abdominal radiology and sees a lot of pancreatic cancer. abdominal radiologists are usually the first who identify the cancer and triage patients to surgeons, gastroenterologists and medical oncologists. “we’re involved in the multidisciplinary care of those patients and we go to what we call tumour conferences where we meet with other specialists to talk about treatment, imaging and the radiology studies that we do on those patients, specifically ct scans [cat scans] and mri scans.”
 11 minute read
11 minute read