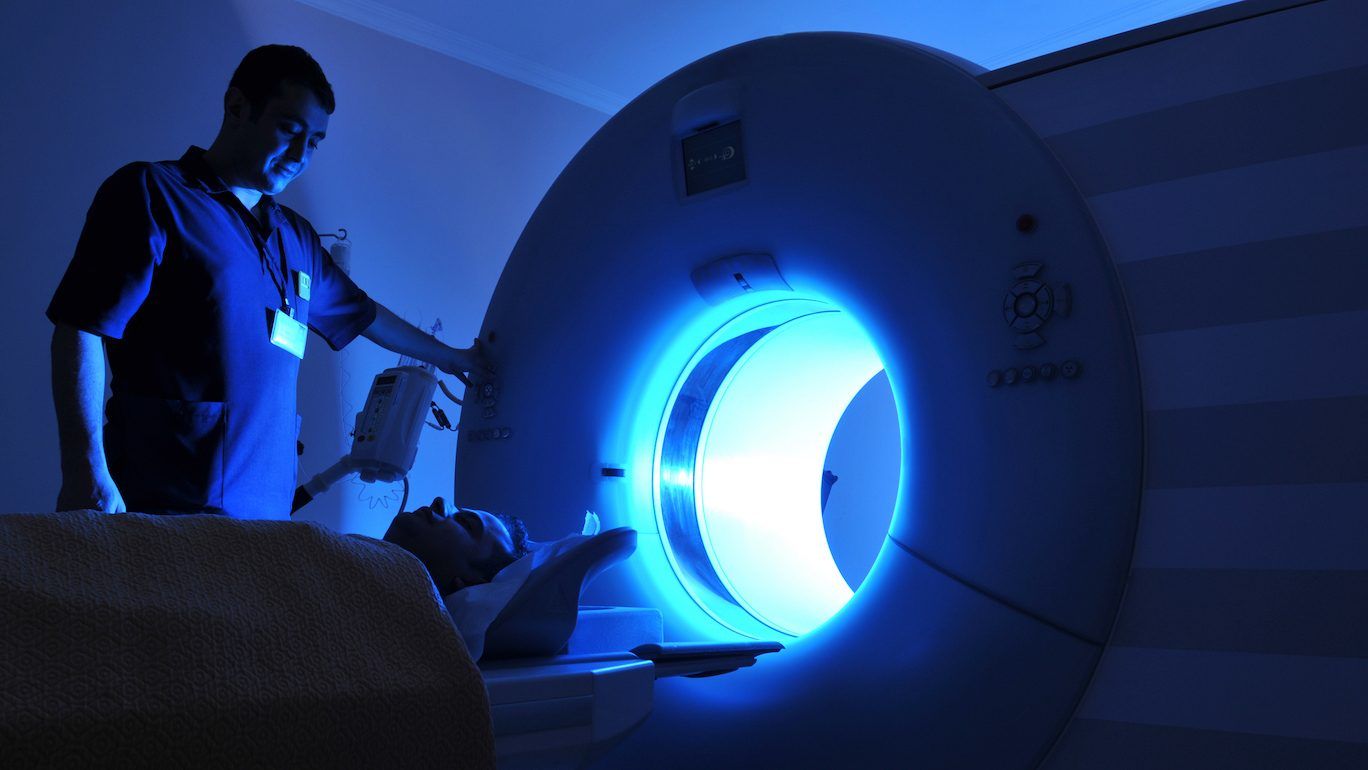
mris reveal ‘significant abnormalities’ in the brains of covid survivors
mris found changes in the frontal lobe and brain stem even six months after patients recovered from covid.
hallucinations, hair loss, erectile dysfunction may be symptoms of long covid
a new large-scale study from the u.k. identifies several troubling new symptoms of long covid.
long covid patients could develop life-long autoimmune diseases like lupus: mcmaster study
researchers say that abnormal antibodies flags the need for long-covid patients to get tested for autoimmune diseases, including multiple sclerosis and type 1 diabetes.
 3 minute read
3 minute read