“the type 1 community is a very strong, fierce family – that’s the best way to put it. they will drop whatever they have, whatever they’re doing to be supportive. the online presence is huge,” she says, grateful for the connections she’s made over the years. “and my door is always open.”
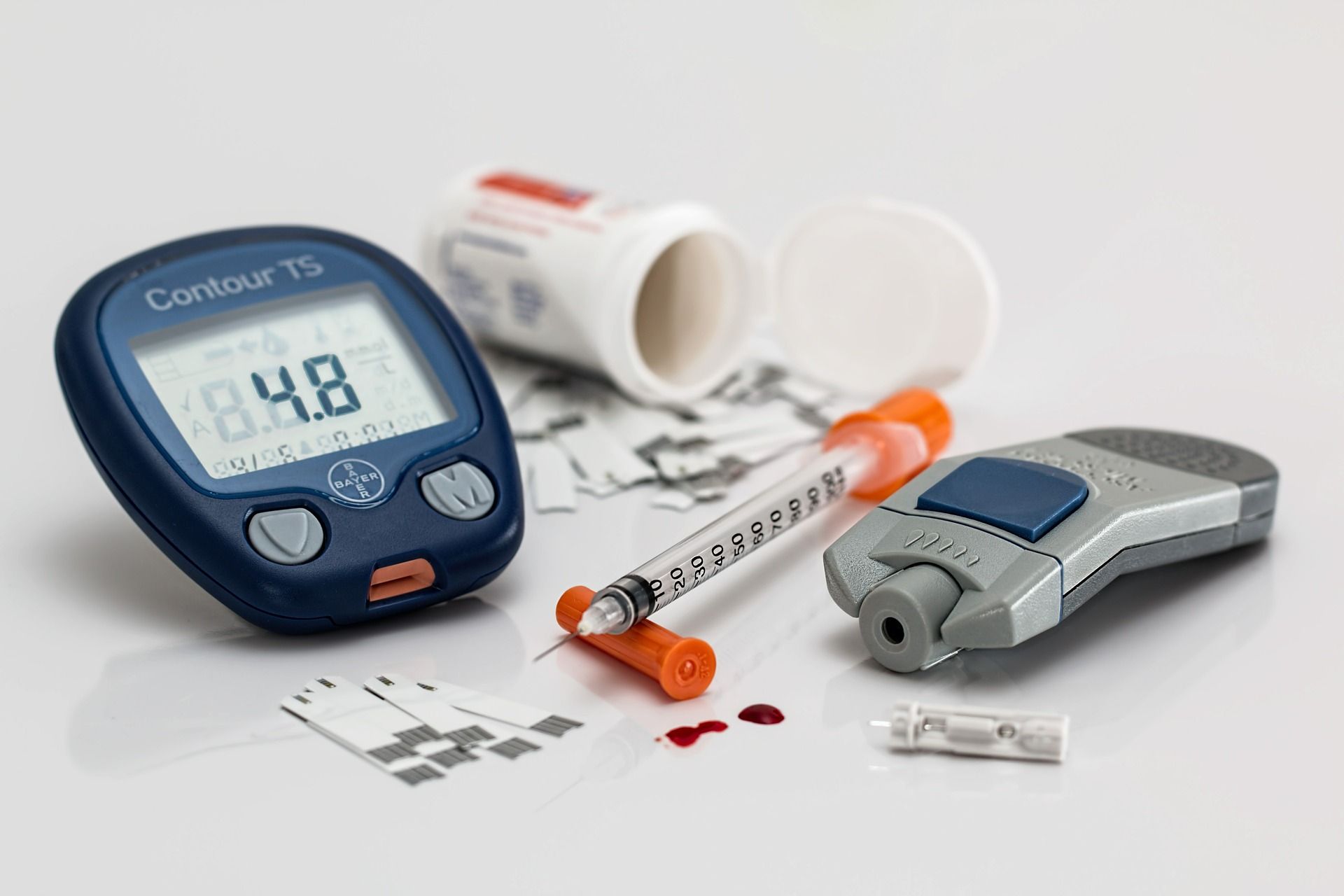
up until two years ago when they were able to qualify for funding support, the family paid thousands of dollars out-of-pocket for mason’s continuous glucose monitoring system, which meant scrutinizing finances and buying 15-year-old vehicles. “in all honesty, there needs to be more access for families that don’t have the means to afford the devices.”
the day-to-day of giving mason the freedom to just be a kid is still a constant challenge. he has a full-day nurse who stays with him at school in the classroom, making sure he’s okay and adjusting his insulin pump dosing if needed because his diabetes is so complex.
when his blood sugar is high, he can get really excited, irritable and argumentative, and when it dips down, he often ends up in tears and quiet frustration.
“type 1 diabetes is incredibly unpredictable. it has no rhyme or reason. how his blood glucose reacts with the exact same activity, no two days are the same. no two moments are the same. so it’s constant and it’s relentless. you don’t have the option to say, ‘i’m tired today, i don’t want to deal with this.’”
 8 minute read
8 minute read