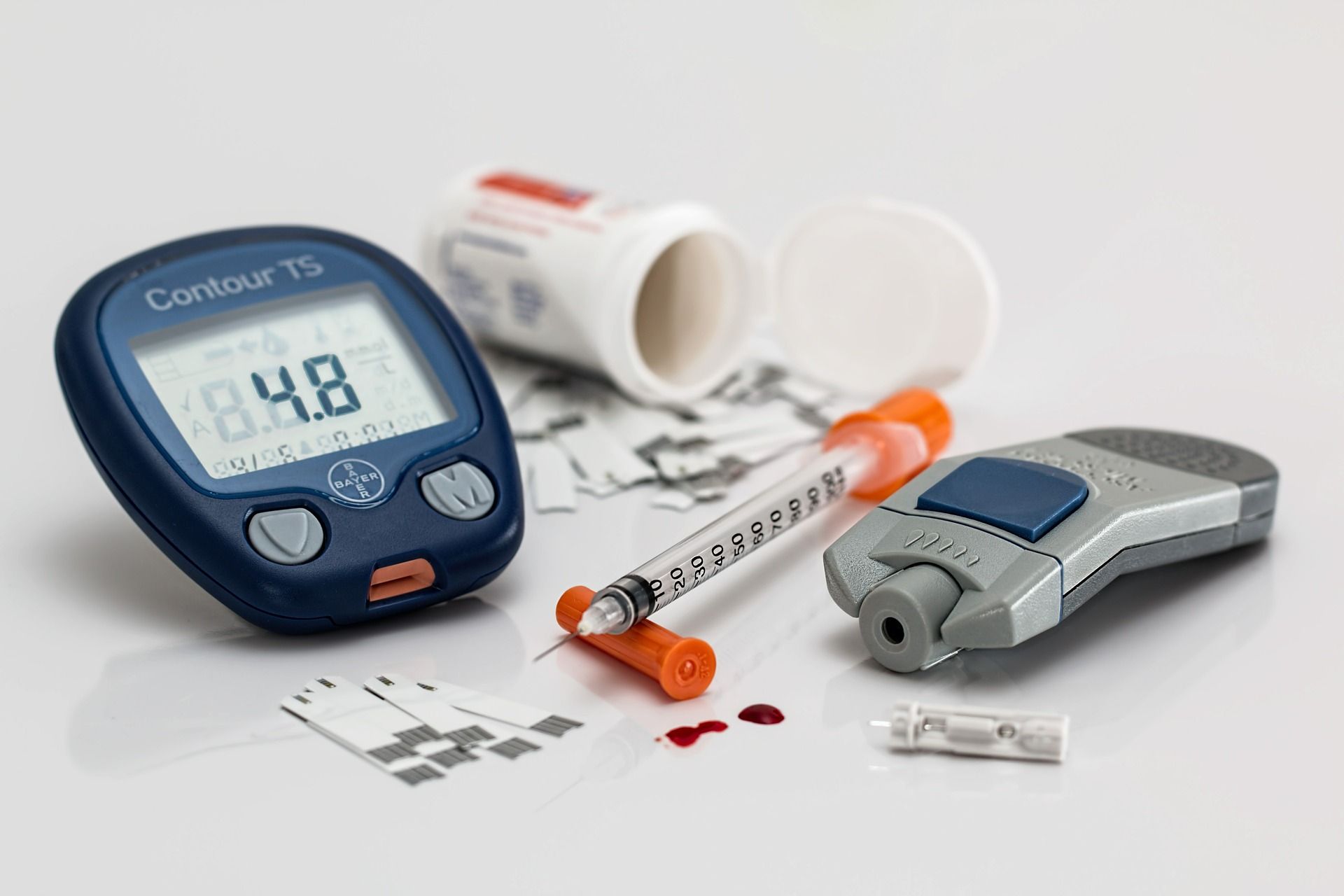
living with type 1 diabetes: my journey through misconceptions, stigma and resilience
living with t1d has made me resilient, and i take pride in the strength it has forged within me over the past three decades.
opinion: the time has come to address and erase stigma surrounding diabetes
despite diabetes being one of the most common chronic conditions in canada, it is loaded with negative perceptions.
world’s first weekly insulin injection available in canada: what this means for diabetes patients
canadians living with diabetes will soon have access to the first-of-its-kind drug, awiqli, a long-acting insulin injectable that is taken once per week.
 7 minute read
7 minute read