10 men's health projects movember has funded
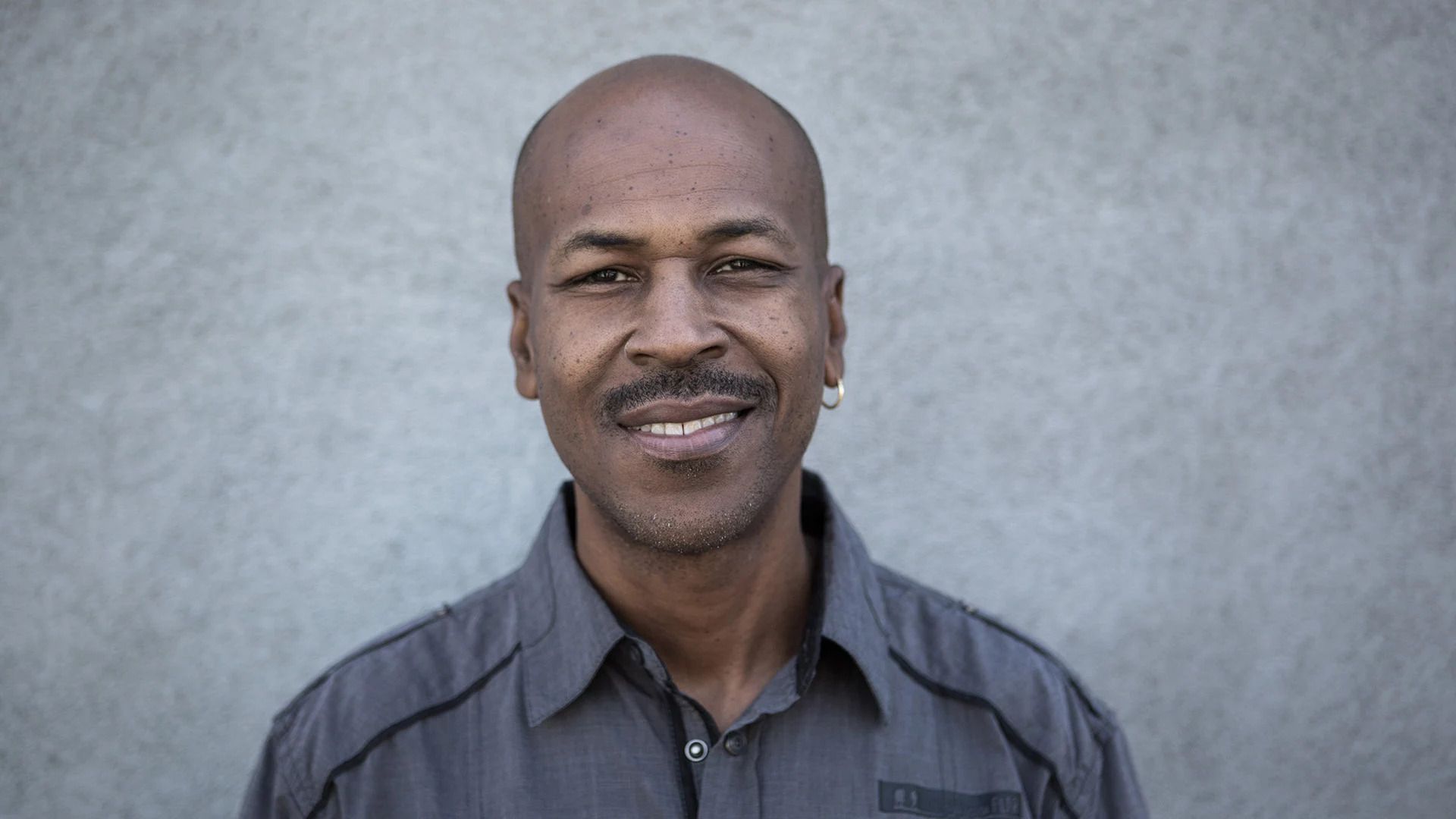
forward momentum increasing diversity in research and resources for men with prostate cancer black men are twice as likely to die from prostate cancer than white men.
forward momentum aims to address racial disparities, increase diversity in research and develop new digital resources for black men with prostate cancer. these new digital resources will be delivered through movember's dedicated prostate cancer website, true north .
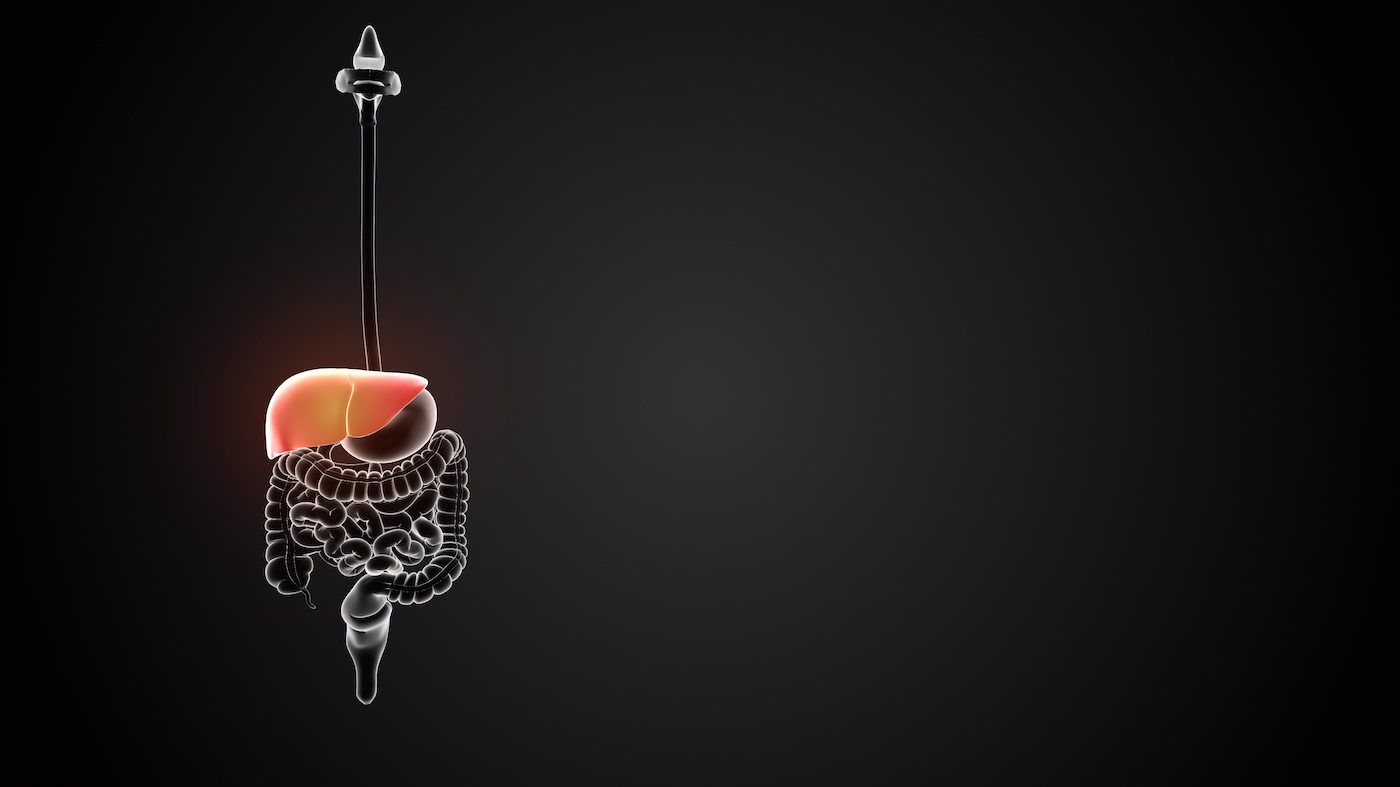
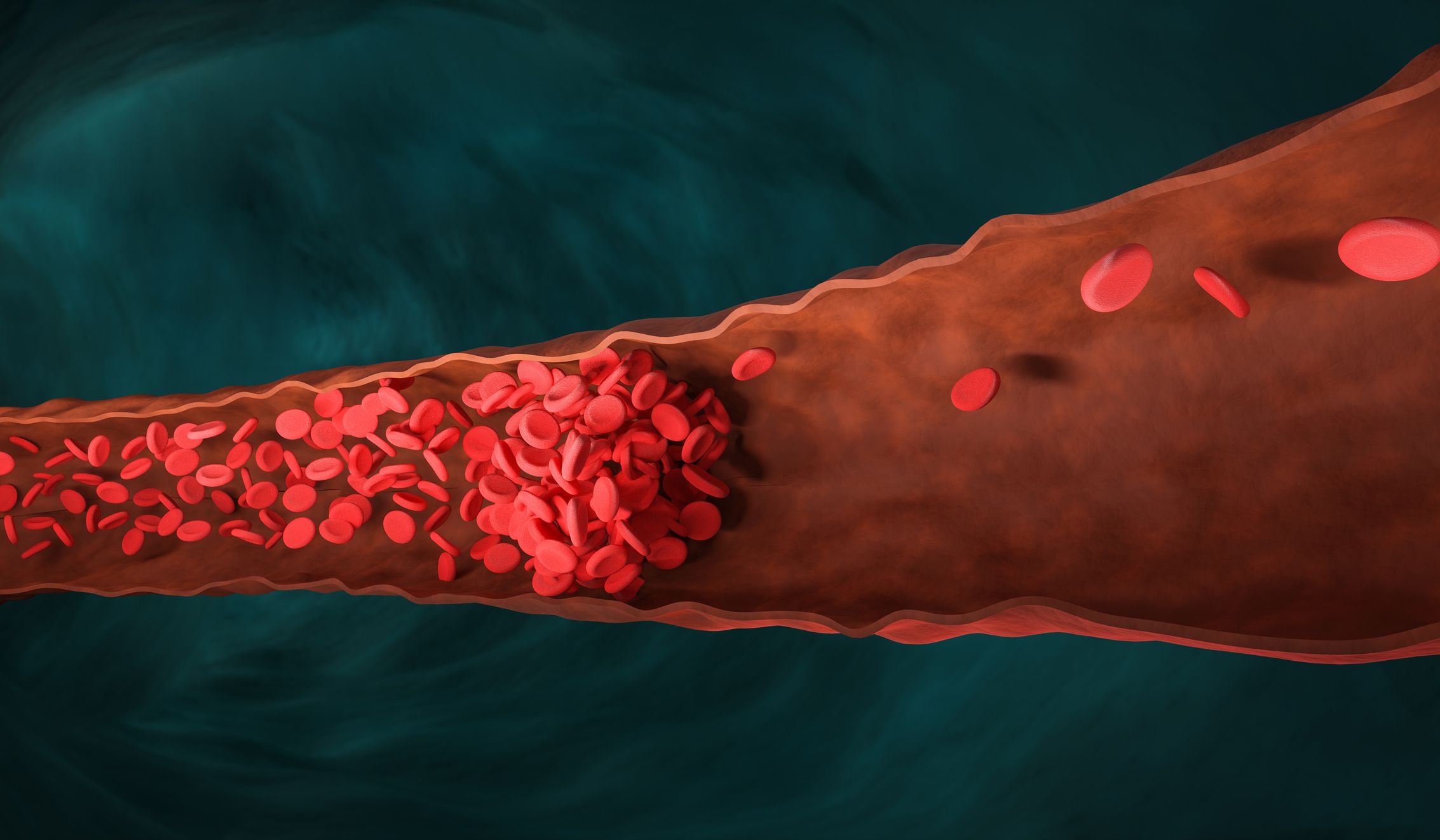
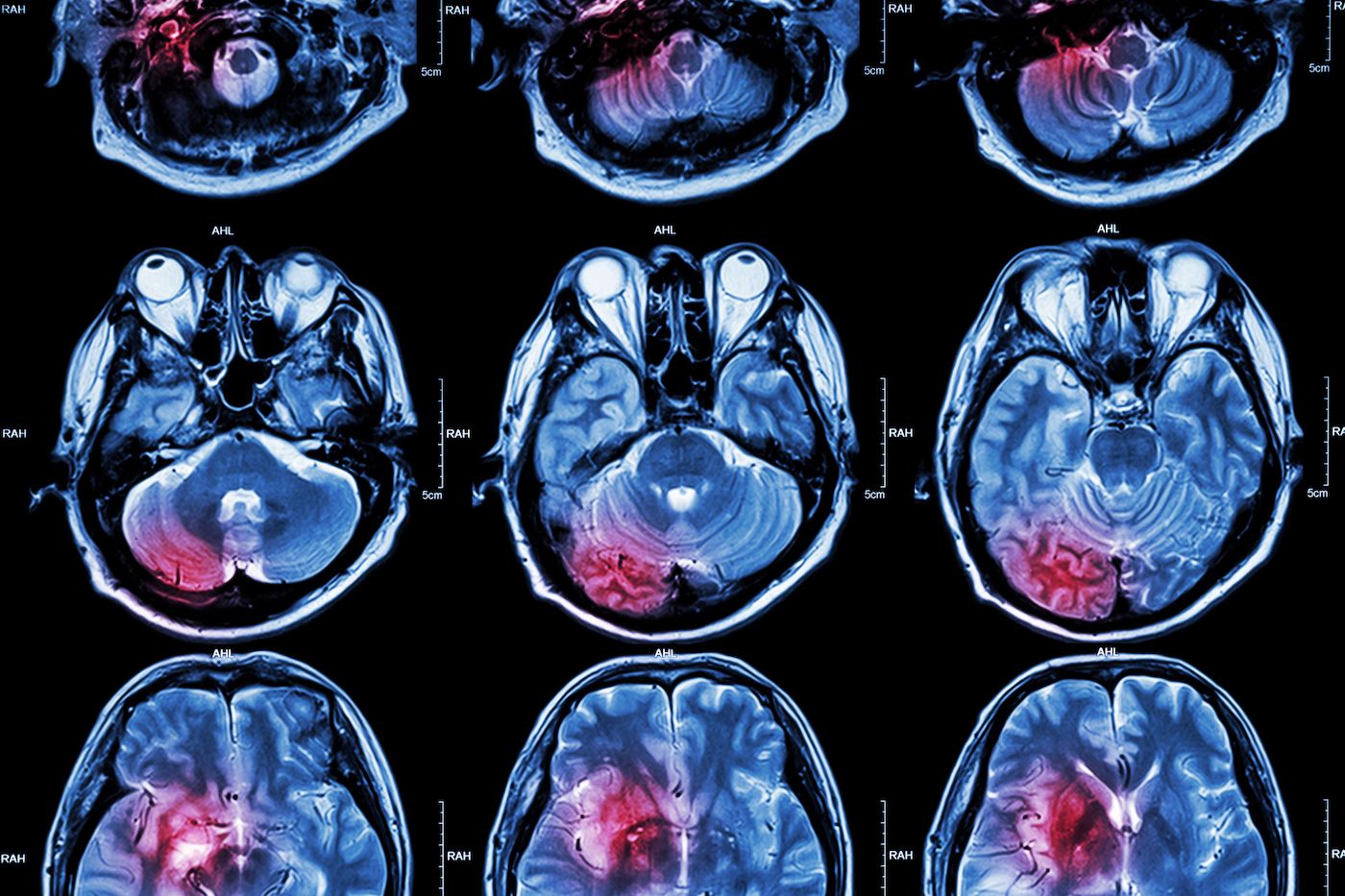
propsma a new type of scan improving accuracy in prostate cancer treatment through a movember-funded study, scientists have developed a new scan that helps doctors understand whether a man's prostate cancer has spread.
making "family" dads' new favourite f-word.
therap trial a new radiotherapy treatment for men with advanced prostate cancer this year, we reached the end of a trial investigating the benefits of a unique radiotherapy treatment for men with advanced prostate cancer called lu-psma. the interim results of the trial showed that lu-psma is more effective than standard chemotherapy for men with advanced prostate cancer.
mental health practitioner research helping us learn more about gendered mental health care the number of men seeking out mental health support is increasing, but the suicide rate remains the same.
movember canada
sep 13 2021