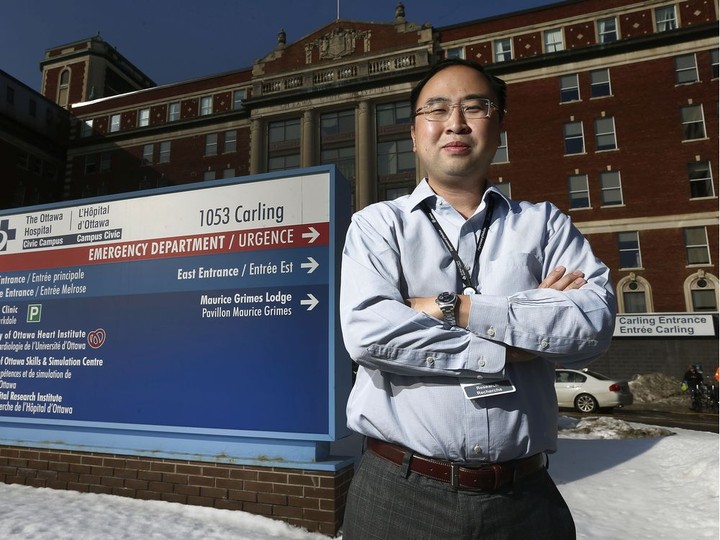
each new long-term care bed costs between $212,000 and $268,000 to develop, said sinha, who is also the director of health policy research at the national institute on ageing at ryerson university.the ndp plan calls for 20,000 beds above and beyond the 30,000 the ford government has already promised. sinha estimates that will cost between $4.25 billion and $5.35 billion. that doesn’t leave a lot of money left over to convert private ltc to non-profit, he said.complicating the matter, most of ontario’s for-profit homes are older structures, built to 1972 standards on prime urban real estate. even if the province revoked their licenses, operators would still own the homes, the fittings and the land. buying them out would be not be cheap.“if you close down a for-profit home, you have to compensate them for however many years they have left on the license. and if you do buy the home, what you’ve bought is something built to 1972 standards,” sinha said.the provincial ndp said it is confident that the amount it would take to overhaul long-term care is sufficient, adding it has consulted with experts in developing the plan.speaking to ontario’s long-term care covid-19 commission in november, health care researcher hugh armstrong said he can’t see the province eliminating for-profit homes in the near future, but he would like to see movement in that direction.unfortunately, ontario is moving in the opposite direction, said armstrong, a distinguished research professor and professor emeritus of social work and political economy at carleton university.the homes being built in the province are largely being built by private equity, with operators getting the money back from government over 20, 25 or 30 years, armstrong told the commission, which is probing how and why covid-19 spread in long-term care homes.borrowing costs are higher for private equity. there’s no reason why government couldn’t borrow at lower cost than private equity and build themselves, said armstrong.“what’s happening now is that here are a lot of new builds being authorized by the province, and they’re overwhelmingly in the for-profit sector, in part because there’s an uneven playing field,” he said.but armstrong also suggested that there may be an opportunity for the province. because for-profits now have a “relatively bad reputation,” the cost of taking them over would likely be lower, he told the commission.alternativesthere may be ways to improve long-term care without converting for-profit homes into not-for-profit. increasing the amount of care residents receive per day is one idea that governments have already embraced. queen’s park announced in november that it is expanding the hours of direct care for each long-term care resident to an average of four hours per day, up from two hours and 45 minutes a day.targets have been set to reach the new standard by 2024-25. it will likely cost $1.52 billion, in 2020 dollars, to meet the standard across ontario’s 79,000 long-term care beds.more transparency in the system could also improve care. in the u.s., for example, every facility is given a score based on factors such as the number of falls and bedsores. when operators know they are being monitored on quality indicators, they are likely to try and perform well, said the ottawa hospital research institute’s tanuseputro. it could also have unintended consequences, depending on the what is measured: some indicators, such as falls, are easy to disguise by restraining residents and putting them in wheelchairs.“we need to look at those quality indicators, but they are fraught with potential issues,” tanuseputro said. “you can’t fudge hospitalizations and deaths.”for example, a “proxy measure” for quality of care is the proportion of residents who get certain medications while they are dying, tanuseputro, who is a palliative care physician, said. every dying patient will lose the ability to swallow. the question is whether they are administered subcutaneous pain relief in the last two weeks of life. this is only possible in homes that are adequately staffed, he said.accreditation is another measure that could close many loopholes, sinha said. it’s a way for organizations to demonstrate to the public that they are upholding international-recognized standards on quality, safety and people-centred care. it involves self-assessments by the organization and on-site surveys with peer reviewers.all hospitals in the province are accredited by accreditation canada, but it’s not mandatory for long-term care, sinha said. in ontario, 98 homes — about 16 per cent of the province’s total — are not accredited. only about 30 per cent of not-for-profit homes are accredited, he said.a long-term-care insurance program, similar to the canada pension plan, may also be worth exploring, saidstamatopoulos, the caregiving researcher from ontario tech university.germany, the netherlands and japan all have programs using various models. the insurance plan can fund home care or long-term care, depending on the recipient’s needs.the province could also consider paying families to take care of their ailing relatives at home, rather than admitting them to long-term care facilities.perhaps the most audacious solution of all is to eliminate the reliance on long-term care homes and replace them with reliable home care and small group home-like residences, an approach denmark has taken, patricia spindel, one of the co-founders of social action ontario, said.canada spends $6 on institutions for every $1 spent on community care, which is one of the most unbalanced approaches in the oecd, spindel said.whether an institution is for-profit or not-for-profit, it’s still an institution and no one wants to be in one, she said. “the whole system is set up in a way that doesn’t make any sense — 85 per cent of families would choose a different situation if there was a different option.”whatever the solution, the clock is ticking. as the population continues to age, the costs of long-term care for the elderly is a moving target. if public policy continues on its current track, public sector long-term care costs in canada will more than triple by 2050, from $22 billion to $71 billion, according to an estimate by the university of ottawa’s wolfson and his colleagues.they are also predicting increased pressure on unpaid caregivers, which will need to increase their efforts by 40 per cent, while the number of canadians using such care is projected to rise by 120 per cent.the system has about 15 years to gear up to the increase in demand, said wolfson. “this is only the tip of the iceberg. the oldest baby boomers are just reaching their 70s.”coyle, whose mother died after a stay at the for-profit almonte country haven, believes that covid-19 will be a catalyst for transformation in long-term care. “i recognize that this is going to be a very long process. there are a lot of things that need to happen to improve,” she said.unlike 20 per cent of ontario’s long-term care homes, almonte country haven now has a family council, where families are working on building more collaborative relationships with the facility.“if we don’t use this to change a system that has been in need of change for a long, long time, it will be a travesty.”by the numbers623: number of ltc homes in ontario360: number of for-profit homes162: number of not-for-profit homes101: number of municipal homes75,676: number of ltc residents in ontario, mar. 29 to may 20, 202079,000: number of licensed ltc beds in ontario38,000: number of people on the waitlist for a bed30,000: number of ltc beds the current provincial government has pledged to build in the next 10 years26,531: beds in ontario ltc homes whose licenses will expire on june 30, 202581 per cent: proportion of covid-19 deaths in canada that were ltc residents, according to a canadian institute for health information report on june 25, 202027 per cent: proportion in england and wales28 per cent: proportion in australia31 per cent: proportion in the u.s.34 per cent: proportion in denmark and germany49 per cent: proportion in sweden66 per cent: proportion in spain53.6 per cent: proportion of private-sector care homes in ontario that have older design standards18.5 per cent: proportion of not-for-profit homes11.9 per cent: proportion of municipal homes$12.74-$16.1 b: cost of building 30,000 new ltc beds and redeveloping 30,000 existing beds, according to the national institute on ageing$187,336 to $216,993: capital infrastructure costs associated with developing or redeveloping a ltc bed$19,214: new costs, per resident per year, being proposed to support the ontario government’s plan to provide at least four hours of direct care a day by 2024-25$4.6b: amount ontario budgeted for ltc in 20207 per cent: proportion of the total health budgetthe cost of long-term care$184.96: minimum cost of ltc, per resident, per day$102.34: amount per day spent on nursing and personal care$12.06: amount per day spent on specialized therapies, recreational programs, and support services$9.54: amount per day spent on raw ingredients used to prepare meals$56.52: amount per day spent on “other accommodations” such as housekeeping services, buildings and property operations and maintenance, dietary services, laundry and linen, general and administrative services, and facility costs$4.50: amount per day for “additional global per diem,” which may be spent on any of these four envelopes. up to 32 per cent may be allocated to the “other accommodations” envelopeat least $62.18: how much residents are expected to pay, per day, out of their own pockets for basic accommodations35 per cent: proportion of ontario ltc home residents who receive financial assistance form the province to cover these costs
share story
share this story
can for-profit care homes be switched to the non-profit model?
 17 minute read
17 minute read