deonandan: wearing a mask is still helpful, but choose a good one
if you can, select a respirator mask over the cloth variety, and limit the time you spend indoors with people who might be infected.
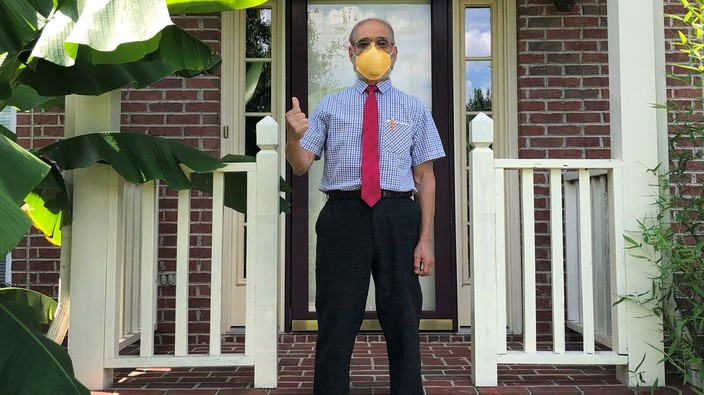
peter tsai, the inventor of the filter material used in n95 masks, is shown at his home in knoxville, tenn. during the pandemic, the materials scientist came out of retirement to help with respiratory mask shortages.
kathy tsai
/
pst
it seems so long ago now, but it was late in 2020 when ontario first made masks mandatory in all indoor public spaces. back then, most public health leaders believed that covid-19 was most commonly spread through large exhaled droplets that fall to the ground within a couple of metres. that’s why we had physical distancing, to keep people out of others’ droplet zones. a simple cloth mask would then serve as a kind of “wind break,” trapping those droplets just in front of the face and negating the need for distancing. the assumption was that if enough people wore such masks, the overall effect on the population would substantially diminish disease transmission. sure enough, as evidence came trickling in, most of it pointed to measurable covid containment. indeed, when two symptomatic, infected hair stylists attended to 139 clients, none of them became infected, as the stylists were properly masked.
the scientific consensus on the dominant mode of covid transmission shifted, though, with the majority of experts now convinced that the disease is mostly transmitted via the airborne route, wherein exhaled smaller droplets, or “aerosols,” don’t fall to the ground quickly, but linger in the air for hours and drift over many metres, much like cigarette smoke.
advertisement
this explains why the simple cloth masks, while useful, aren’t as effective as some had expected in curtailing transmission. aerosols can leak through the open tops and sides of baggy cloth masks. but so-called respirator masks, such as the n95 or kn95 types, are fitted to the face for less leakage. clinicians have traditionally had their respirator masks “fit tested,” meaning that the seal around their faces has been tested to ensure a tight fit. this is not necessary for non-clinicians, as non-fit tested n95s are more than good enough for the rest of us.
when talking about masks, it’s important to distinguish between respiratory protection and source control. the former is about protecting the wearer, while the latter is about protecting others from the wearer. simple cloth masks, like surgical masks, are meant to mostly provide source control. (“my mask protects you; your mask protects me.”) respirator masks provide both source control and respiratory protection.
cloth masks aren’t useless in an airborne epidemic, though. when we exhale aerosols, most of it comes out as a plume directly in front of our mouth and nose, where the cloth mask helps reduce its effect. but cloth masks are clearly not as good as respirators in either containing the plume or in filtering out incoming virus particles.
advertisement
in fact, any kind of face covering is preferable to none at all. even the very cheap, low-quality masks you might buy in bulk from the dollar store have some effect, though are not optimal. the important factor to consider is the duration of exposure. the longer the time spent in an indoor setting with persons who might be infectious, the sooner certain masks will allow the wearer to receive an infectious dose.
an analysis by dr. lisa brosseau for the center for infectious disease research and policy showed that if two people near each other are wearing surgical masks and one of them is infected, it takes less than an hour for the other person to receive an infectious dose. but if they’re both wearing non-fit-tested n95s, it would take many hours to receive that same dose.
further, brosseau found that if one were to wear an n95 and were near a completely unmasked infected person — a situation in which many will soon find themselves — it would take about an hour to receive infection. a surgical or cloth mask reduces the time to less than half that.
all masks work, but some masks work better than others. in this new era of relaxed mandates, if you seek continued self-protection, there are two things you can do as you go about your everyday life: choose a respirator mask over a cloth mask, and limit the time you spend indoors with people who might be infected.
advertisement
raywat deonandan is an epidemiologist and associate professor with the faculty of health sciences, university of ottawa. he plans to properly mask indoors with people whose vaccination and infection status are unknown.
n95 face masks are the best, though others can still be helpful.
tobiasone
/
getty images/istockphoto
 3 minute read
3 minute read
