'a lifelong challenge': living with a chronic blood cancer like cml changes everything
while chronic myeloid leukemia is no longer a death sentence for most patients, people like advocates amber noden and theresa harvey say that the side effects of medication have had huge impacts on their quality of life.
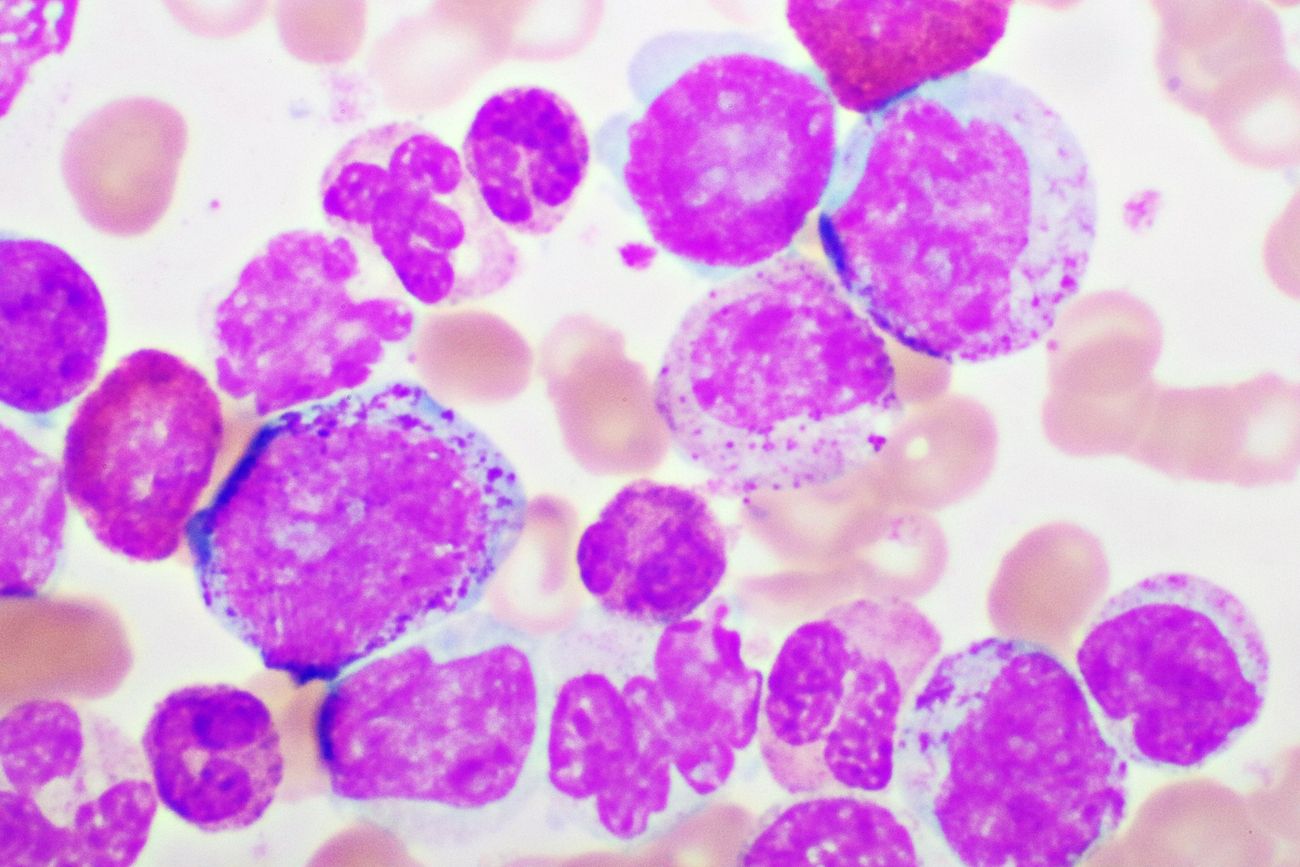
leukemia: do you know the signs?
leukemia occurs most often in adults after the age of 55, but it is also the most common cancer diagnosed in children younger than 15.
shift: i have omicron and an insatiable craving for salt and vinegar chips
'we aren't sure what to expect' is never what you want to hear — not from the person flying your plane, or the contractor renovating your house, or the dude making your first latte of the morning, but especially not from a doctor.
 6 minute read
6 minute read