to drive or not to drive? something to consider after a concussion, brain injury
researchers tested people who had a concussion with a driving simulator and found they were less able to centre virtual vehicles in the lane and allowed the vehicles to hit road shoulders more frequently, especially when negotiating curves

a 2017 university of georgia finding showed a negative impact on driving-simulator performances even 48 hours after concussed individuals no longer experience symptoms and medical professionals deem them clinically recovered.
alessio lin
/
unsplash
by: gord holder, postmedia
even casual fans have heard or read references to players being in “concussion protocol” for one sports league or another.that usually means the athlete is sidelined for a week or more while progressing through mandatory stages of recovery such as a rest period, cognitive tests, increasing levels of physical activity and contact and medical or training staff clearance before returning to competition.“return to work” and “return to classroom” protocols exist, too, but what about the act of getting to the arena, gym, office or school?there’s not much more than common sense involved with “return to driving,” so this represents an opportune time to reference a university of georgia finding of a negative impact on driving-simulator performances even 48 hours after concussed individuals no longer experience symptoms and medical professionals deem them clinically recovered.these “drivers” are less able to centre virtual vehicles in the lane and allowed the vehicles to hit road shoulders more frequently, especially when negotiating curves, the 2017 study found.a followup study of student-athletes with reported concussions says most of them will not stop driving at any point, even though they believe it’s unsafe to drive immediately following a concussion. more than one in three say driving restrictions will “definitely” or “probably” influence decisions to report brain injuries to health-care providers.“it would be really easy to say, ‘that’s simple. let’s just say anybody with a concussion cannot drive until their symptoms go away,’” says julianne schmidt, lead author for both studies and an assistant professor in the university’s kinesiology department.“but we have to think about the negative consequences that could actually deter people from seeking care to begin with, which is already a surmountable problem that we face in sports medicine. just to get them to come in the door at all is a challenge, so we have to think about the negative consequences of what extensive driving restrictions mean.”ontario ministry of transportation provisions revised in 2018 require physicians, nurse practitioners and optometrists to report “certain high-risk medical conditions, functional impairments and visual conditions,” including cognitive impairment, sudden incapacitation, motor or sensory impairment, visual impairment, substance-use disorders and psychiatric illness.advertisement

dr. julianne schmidt stands as graduate student michelle weber demonstrates use of a driving simulator as part of a study led by dr. schmidt into the effects of concussions on an individual’s ability to drive a motor vehicle. dr. schmidt is an assistant professor in the department of kinesiology at the university of georgia in athens, ga.
university of georgia
in assessing fitness to drive, a spokesman adds, the ministry relies on those regulations and on canadian council of motor transport administrators national standards that list concussion as a “transient” or temporary impairment with no likelihood of recurring episodic or ongoing persistent impairment.“depending on the severity of the concussion, however, some practitioners may choose to report the condition if they are of the opinion that the person poses a risk while driving,” the ministry’s statement adds. “where significant cognitive or motor/sensory impairment is noted, a licence suspension may be issued.”dr. jamie dow of the société de l’assurance automobile du québec says someone who has a concussion should probably not drive for at least another day or two, when they no longer have headaches and normal neck movement returns, but the provincial auto insurance agency isn’t concerned about a temporary condition that should resolve itself in 48-72 hours.however, quebec’s highway code also requires all drivers to demonstrate that, despite any incapacity, they can still drive correctly.“the problem for many people is nothing important happens when they’re driving, so they’re on autopilot or they’re thinking about 101 other things, whatever it is. they’re listening to the radio, singing along …,” says dow, saaq’s medical spokesman.“but, when you are not ill or you don’t have a problem, if something happens, you can stop whatever you’re doing and you have the reserves to be able to cope with any emergency, we hope.” however, distracted driving is still a major cause of accidents or crashes.“but i think it’s common sense that, if you’re not feeling well, then you’re probably better off not driving, just in case something happens that you have to respond to rapidly. after a concussion, you’re not thinking normally. you’re slower, mainly, and, when you’re on the road, you don’t have more time to handle an emergency because you’re not feeling well.”

physiatrist dr. shawn marshall at the ottawa hospital general campus often works with patients who need treatment for concussions, and some who might end up using the caren system tilting treadmill platform with a 180-degree screen displaying a variety of virtual scenes, game modes, and sometimes simple math problems to assist in cognitive rehabilitation.
david kawai
/
ottawa citizen
advertisement
multi-tasking at 100 km/h
dr. shawn marshall says patients frequently ask him if they can drive after a concussion or other more serious brain injury.the answer is usually “yes,” says marshall, the division head for physical medicine and rehabilitation at the ottawa hospital, but he adds that he reminds every driver they’re responsible for being fit for driving.marshall, who has research affiliations with university of ottawa brain and mind research institute, ottawa hospital and bruyère research institute, compares concussion impairments to those for alcohol or marijuana: having a drink or smoking a joint is legal, but an individual is temporarily impaired from driving because they’ve decided to do that.immediately after an acute concussion, an individual is not fit to drive, marshall says, and anyone with a concussion is cognitively affected in three areas, which are all relevant to driving:• information-processing speed, or how quickly they take in information and use it;• dividing their attention between tasks like checking the speedometer, then looking down the road and refocusing on the rear-view mirrorz
• ability to focus.“guess what’s really important for driving?” marshall says. “well, the ability to multi-task and the ability to take in information quickly. you’re moving at 100 km/h. our bodies weren’t made to move at 100 km/h. information is coming to you, your focal point is changing at 100 km/h. we fully don’t understand how much brain power it’s using.”

this is a screen shot from the simulator used in a study about concussions and the impact they can have on an individual’s ability to drive a motor vehicle.
advertisement
many possible signs
dr. charles tator, director of the canadian concussion centre in toronto, told a hearing of the house of commons subcommittee on sports-related concussions in february that canadians reported 200,000 concussions annually.and most people with concussions don’t show up at physician’s offices or emergency rooms, says blaine hoshizaki, director of the university of ottawa’s neurotrauma impact science lab. even if they know they’ve taken hits to the head and experience headaches or confusion, they often don’t link those factors. “because the signs or symptoms are so inconsistent, if they got hit in the head, they have to be aware of all the signs, any sorts of inconsistency with vision, balance,” hoshizaki says. “i think there’s probably close to 60 symptoms, so, if you hit your head and you recognize any of these, then you should be concerned because the problem we have is that driving is a pretty complex thing that we kind of learn to do almost automatically.“so, how that influences awareness alone, knowing that there’s a person in your blind spot, that’s a pretty subtle sort of cognitive responsibility, that you’re driving along and you’ve seen a guy and you know he’s driven up into your blind spot. if you’re cognitively compromised, that little thing might miss …“there are so many elements to how your brain functions that it’s almost automatic, that you won’t necessarily pick up when you’re missing it.”
advertisement
individual differences
schmidt says other conditions such as severe traumatic brain injury (tbi), stroke or parkinson’s disease aren’t as transient as concussion, which means they won’t go away and are easier to identify, which in turn eases the process of getting an individual into disability services.concussions typically require 10- to 14-day restrictions, schmidt adds, but the unknown is exactly how long concussion-related impairment lasts beyond symptoms, and what about potential differences based on age, gender or other demographic factors?“we used college-age athletes and non-athletes — mostly non-athletes — but what does this look like in your 16-year-old adolescent driver? what does this look like in your 50-year-old driver,” schmidt says. “concussion recoveries can differ quite a bit in those groups, as well.“so, i don’t have an answer for you, but i’m curious about the same thing.”significant in daily life
dow says medical personnel examining a patient with a possible concussion or head injury often start out by asking that individual if they can move their fingers or hands or having them count backwards, but they don’t think to tell that person to avoid driving for a few days.medical personnel “tend to forget” that driving is an everyday activity, particularly for canadians who don’t live in major city centres, he adds.to counter that situation, saaq has a workshop for physicians and other health personnel to underline the importance of driving and how it should be considered when they’re talking about the impact of whatever has happened on a patient’s life.to be fair, hoshizaki says, evaluating incapacity after a concussion is difficult even for specialists, so imagine the dilemma of a layperson trying to figure out if he or she is ready to return behind the wheel.physicians can provide guidance, hoshizaki adds, but there’s no real way of telling people they can’t drive.“when we talk about guidelines to return to play or (other) guidelines, they’re guidelines,” he says. “they’re not rules.”dow says the process of removing a driver’s licence takes about six weeks, so, effectively, saaq tells quebec physicians to report conditions only if the consequence of previous injury or disease — formally called “sequelae” — last six months or more. as one example, he refers to a former municipal transit driver who, following a severe concussion, functioned at the cognitive level of an eight-year-old.“temporary” conditions such as concussions do not have to be reported to provincial authorities unless they affect driving and a patient says he’ll drive anyway.“the point is, if you were advised by your physician not to drive and you do drive and you kill somebody, you can be liable for accidental homicide, which is something you have to bear in mind,” dow says. “you’re also going to have that on your conscience for the rest of your life.”looking for biomarkers
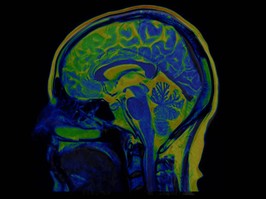
it would be easier to advise someone not to return behind the wheel after a concussion based on specific medical indicators or “biomarkers,” but nobody has figured that out, despite what hoshizaki describes as “a fair bit of money” invested in research in canada.there are known biomarkers for brain injury, marshall adds, but, because brain injury is a spectrum, even those biomarkers are not useful enough in diagnosing concussion.similarly, magnetic resonance imaging (mri) or diffusion tensor imaging (dti) scans can reveal signs of concussion, but marshall says that again they are neither sensitive nor specific enough to be gold-standard tests for diagnosing concussions. in other words, they could miss diagnosing concussions at the individual level, which is a clinical diagnosis anyway.the ideal, schmidt says, would be to use current clinical tools to predict or find patient patterns differentiating between someone who shouldn’t drive and someone who could.“even though they both have a concussion, maybe you’re having issues with reaction time, and we know that is a better predictor, better indicator of your driving safety,” she says. “however, you’re having more issues with your memory, which might not be as related to your safety in driving. it might hurt your ability to navigate in driving, but you’re ok, your safety on the road is fine …“my second preference, then, if that’s not possible because it’s possible that the clinical tools we use now don’t predict those things very well or are not sensitive enough to those things that they wouldn’t work in that way, would be then to introduce a new tool or assessment battery that was short and succinct, but got at someone’s readiness to return to driving so that, clinically, we could return them to driving as soon, as quickly, but as safely as possible.”out of the dark
guidelines to concussion management have changed, with “return to activity as tolerated” as a general counsel.marshall says “return to sport,” is easy since concussed athletes simply must go through established protocols and show themselves to be symptom-free because they’re otherwise at increased risk of injury.“return to school” is hard, he says, because it’s a distracting environment requiring cognitive and social energy, soa concussed student might have to start off by avoidinggym or taking only one class.for driving, perhaps a 10-minute commute would be ok, but not a long vacation trip, says marshall, who likens it to recovery from a sprained ankle: if you can walk without pain, proceed, but, if walking causes pain, back off temporarily before trying again.“obviously, if the person is acutely confused and doesn’t know the date or doesn’t know where they are, they shouldn’t be driving. most of us would say that,” he says.“we used to say, ‘go into a dark room and wait for your symptoms to get better.’ they tell them not to do that now. now they say, ‘after the first 24 to 48 hours, return to activity as tolerated.’ and, if you return to activity as tolerated, that would mean you get to make decisions on what you can handle and can’t handle.”gholder@postmedia.comtwitter.com/holdergord
 9 minute read
9 minute read